Though it may sound like the title to a straight-to-DVD sci-fi movie, Alien Hand Syndrome (AHS), sometimes referred to as Alien Limb Syndrome, is a true disorder that it quite horrific and troublesome to those who suffer with it. This rare disorder is neurological in origin. The “alien” hand functions involuntarily without the owner’s awareness of its actions. Some of the lesser symptoms associated with AHS are involuntary grasping, pulling at clothing, and reaching or touching ones face. Some of the more serious symptoms are self-inflicted choking or pinching, inhibiting the “normal” hand from implementing tasks, and involuntarily forcing food into the owner’s mouth.
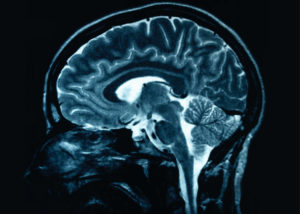
AHS was first documented in 1908 by Neuropsychiatrist, Kurt Goldstein. It is theorized by some that the cause of AHS is traumatic brain injury or lesions to the thalamus, supplementary motor cortex, posterior parietal cortex, anterior cingulate, anterior prefrontal cortex, or the corpus callosum. Several more believe they have linked AHS to a disconnect between differing sections of the brain that are responsible for conscious body movements. Others, however, hypothesize that the release of the primary motor cortex from conscious control is behind the unwanted or unplanned movements. Nonetheless, the exact cause of the neural contrivances has not been definitively identified.
 There are “subtypes” of AHS which are linked to injuries/lesions in specific regions of the brain. The subtypes are callosal variant, frontal variant, and posterior variant. The callosal variant is usually associated with agonistic dyspraxia and diagnostic dyspraxia. Agnostic dyspraxia is the involuntary movements of the alien hand (AH) when commands of movement are given and made by the unafflicted hand (UH). An example would be a patient being told to touch their nose with their UH and their AH would involuntarily follow the action as well. Diagnostic dyspraxia is the interference by the AH in the actions of the UH. Good example of this action would be a patient trying to stir a pot and the AH trying to put a lid on the pot at the same time.
There are “subtypes” of AHS which are linked to injuries/lesions in specific regions of the brain. The subtypes are callosal variant, frontal variant, and posterior variant. The callosal variant is usually associated with agonistic dyspraxia and diagnostic dyspraxia. Agnostic dyspraxia is the involuntary movements of the alien hand (AH) when commands of movement are given and made by the unafflicted hand (UH). An example would be a patient being told to touch their nose with their UH and their AH would involuntarily follow the action as well. Diagnostic dyspraxia is the interference by the AH in the actions of the UH. Good example of this action would be a patient trying to stir a pot and the AH trying to put a lid on the pot at the same time.
The frontal variant subtype is almost always associated with injury/damage to the frontal lobe. The actions of the AH with this subtype are involuntary grasping, reaching, and other purposeful movements. Often times, these movements can also be exploratory as the AH seeks an external object to grasp. Once an object has been grasped, it is extremely difficult for the patient to voluntarily release the item. They may have to resort to prying or peeling their fingers away from the item. These grasping actions can and do take place without the patient even noticing that it is occurring. Many who suffer from this subtype choose to bind or restrict the movements of the AH.
The posterior variant subtype is most usually associated with injury/damage to the occipital lobe and/or the posterolateral parietal lobe. The actions of the AH of this type are quite different from the frontal variant form. These movements tend to be more like pulling away or withdrawing the palm of the hand from contact to any surface. Any contact to that palm is undesirable. The AH will generate movements and actions to prevent or eliminate the contact all together.
Presently, the exact cause(s) of AHS is unknown. Thus, a cure for the syndrome has not been developed. Continued research to identify the correct theory/theories or exact cause as well as a functional treatment are needed.
Work Cited
Alien hand syndrome. (n.d.). Retrieved June 13, 2016, from http://www.medicinenet.com/script/main/art.asp?articlekey=12655
Harris, S. V. (n.d.). Alien Hand Syndrome sees woman attacked by her own hand. Retrieved June 13, 2016, from http://www.bbc.com/news/uk-12225163
Mark, V. W. (n.d.). Alien Hand Syndrome. 5th Annual International Conference on Education & E-Learning (EeL 2015). doi:10.5176/2251-1814_eel15.8
Crystal Bray
WKPIC Doctoral Intern
