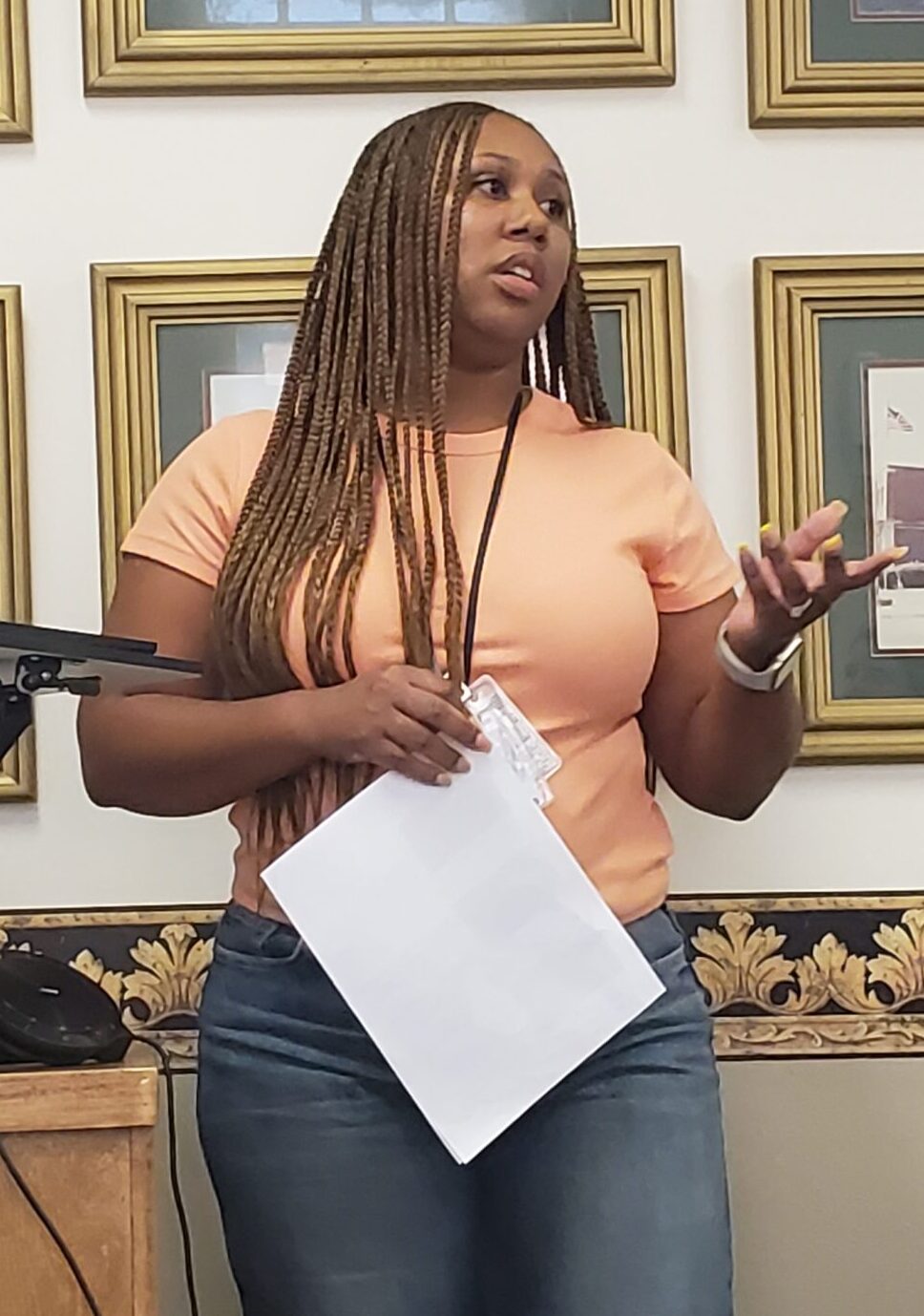
Journical Club- Shakeira Frye
Article: Kip, K. E., Berumen, J., Zeidan, A. R., Hernandez, D. F., & Finnegan, A. P. (2019). The emergence of accelerated resolution therapy for treatment of post‐traumatic stress disorder: A review and new subgroup analyses. Counselling and Psychotherapy Research, 19(2), 117-129.
Purpose: This article discussed the effectiveness of Accelerated Resolution Therapy (ART) for treating individuals with Post-traumatic Stress Disorder (PTSD), specifically among military personnel and individuals with traumatic brain injury (TBI). The article described PTSD as a chronic, disabling psychiatric disorder that is characterized by being exposed to actual or threatened death, serious injury or sexual violence that leads to persistent re-experiencing of the details associated with the traumatic event, avoiding stimuli that evoke thoughts or feelings about the event, negative changes in cognitions and mood related to traumatic event. The article emphasized ART’s potential as a reasonable, shorter alternative to traditional PTSD treatments, especially for military populations with difficult clinical presentations.
What is ART: ART therapy was described as an emerging trauma-focused psychotherapy that is brief relative to other treatments. This article aimed to describe the ART clinical protocol and the theoretical foundations. The protocol consists of four primary steps which included Relaxation and Orientation, Imaginal Exposure, Imagery Rescripting, and Assessment and Closeout. In the Relaxation and Orientation step, the client identifies and states the specific traumatic event they want to address. Next, the therapist directs the patient to focus on their bodily sensations while also performing a set of eye movements. In the Imaginal Exposure step, the client is directed to begin visualizing the traumatic event in their mind from start to finish while also performing eye movements. Again, the therapist asks the client to pay attention to any somatic, emotional, or physiological sensations that they may be experiencing. Those sensations are then processed with a set of eye movements until they are comfortable returning in their mind to the place they left off in the traumatic event. This step is completed when the client can visualize their experience from start to finish two times. The third step, Imagery Rescripting, involves the client being directed to imagine a new and preferred way of visualizing their experience while performing eye movements. The final step, Assessment and Closeout, includes reinforcing techniques which are used to assess if there are any areas of the traumatic event that still causes the client to generate visceral responses.
Study and Results: This study consisted of 291 participants who received at least one session of ART across four studies. The participants were classified based on their TBI status (no TBI, mild TBI, moderate TBI or severe TBI). The participants also had to have symptoms related to PTSD. The results of this study indicated that there were significant reductions in PTSD symptoms among participants. On average, the participants showed a 20.6-point reduction on the PTSD Checklist (PCL) after ART treatment, with 60.8% experiencing a clinically meaningful reduction of symptoms. Among the military personnel with TBI, the response rates to ART were similar regardless of TBI severity.